Cataract surgery is currently the most commonly performed surgery in the world, as about 19 million cataract surgeries are performed globally each year. Presently, the main surgical method is phacoemulsification which involves a 2.5mm incision by a special knife at a region close to the sclera into the transparent tissue at the frontmost part of the eye called the cornea. A gel is injected into the eye, then the front membrane of the optic lens is circularly removed by using very fine forceps. Next, the titanium tip of the handpiece of the phacoemulsification device that vibrates at ultrasonic frequency is inserted into the eye.
The optic lens is liquefied by these high frequency vibrations and sucked out. Following this process, an artificial intraocular lens is inserted into the cleaned capsule. Another method is phacoemulsification supported by a femtosecond laser.
Femtosecond lasers were initially used in refractive surgery in 2001, however only recently have they been improved enough to be employed in cataract surgery. The aim of this technology is to improve the reliability, accuracy and clinic outcome of surgery. Laser energy absorbed by the target tissue creates a plasm consisting of free electrons and ionized atoms, which rapidly expands to create a cavity inside. Subsequently, this cavity bursts to develop a separation in the tissue. Conversion of laser energy into microscopic energy is called photodisruption. All these events occur at microscopic levels. In order to perform laser treatment, firstly an interface is required to transmit laser energy to the eye. The process of providing contact is called docking. In transmission, fluids or lenses are used. The second crucial step is imaging.
Cataract surgery requires 3D imaging since the treatment is performed on a spatial domain rather than a single plane like the case is in LASIK. This is realized by a method called the spectral-domain OCT or 3D reconstruction of confocal image. Centralization of the cornea during the procedure is crucial. If centralization is not performed well, all procedures starting from the incisions will develop outside the desired locations. The cornea should be transparent for the anterior segment to be displayed well. For circularly incising the anterior capsule, firstly the pupillary edge is taken as a reference in centralization and the incision diameter is chosen (typically 5 mm). Then, the lens fragmentation pattern is chosen depending on the hardness of the lens and the preference of the surgeon. This may be a 4,6,8 segment. A safe zone of 500-800 microns at the front of the posterior capsule is submitted to the approval of the surgeon by the imaging system. The pressure due to the vacuuming and applanation applied during docking may cause subconjunctival hemorrhage or intraocular pressure increase. Caution is required in cases with advanced glaucoma and retinal vascular disease. The laser procedure lasts between 30 seconds and 3 minutes depending on the speed of the device and the treatment pattern chosen. Firstly, the anterior capsule is circularly incised, then the lens is fragmented and finally corneal incisions are made. After completing this process, the patient is separated from the laser device and transferred to another bed for phacoemulsification. Surgical cleaning is made. It is possible to wait between the two procedures for a period not exceeding 30-40 minutes. The surgical standard is slightly different from the phaco surgery but in essence, it is the simplified and expedited version of it. During laser application, various problems such as decreased pupil size, vacuum loss and incomplete capsulotomy may arise. On the other hand, the advantages compared to the classic phacoemulsification surgery are correctly located and centralized capsulorhexis at fixed size, lower phaco energy, less fluid circulation and correct and resistant corneal incision architecture. The biggest disadvantage is the approximate additional cost the procedure involves. This system seems to be more effective especially in patients in whom multifocal lenses called premium lenses and/or astigmatism correcting lenses will be implanted.

Figure 1: Docking
In patients in whom astigmatism correcting lenses will be implanted, it is a factor that improves surgical results to use the laser phaco system with imaging systems that record the iris and limbus preoperatively and overlap the images obtained with the live imaging of the surgical microscope. This technology is an important step in improving refractive cataract surgery and a significant development for future techniques and technologies.
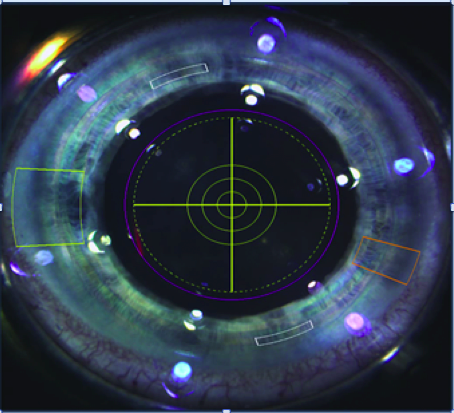
Figure 2: Selection and imaging of incisions
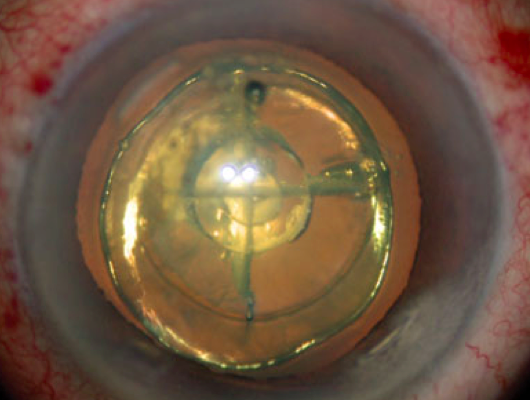
Figure 3: Capsulorhexis and lens fragmentation