 WHAT ARE THE CATARACT?
WHAT ARE THE CATARACT?
Cataract is a clouding of the eye's lens. When we look at something, light rays travel into our eye through the pupil and are focused through the lens onto the retina, a layer of light-sensitive cells at the back of the eye. The lens must be clear in order to focus light properly onto the retina. If the lens has become cloudy, this is called a cataract.
VISION PROBLEMS WİTH CATARACTS
If your vision has become blurry, cloudy or dim, or things you see are not as bright or colorful as they used to be, a cataract may have developed in one or both of your eyes. Many people say that their vision with cataracts is similar to the effect of looking through a dirty car windshield.
As a cataract slowly begins to develop, you may not notice any changes in your vision at first. But as the cataract progresses, you may begin to find that it interferes with your daily activities. Performing a complete eye exam, your ophthalmologist (Eye M.D.) can tell you whether cataract or another problem is the cause of your vision loss.
While cataracts are one of the most common causes of vision loss, especially as we age, they are treatable with cataract surgery. Since most cataracts are part of the normal aging process, they cannot be reversed. There are no medications or eye drops that will make cataracts go away—surgery is the only treatment.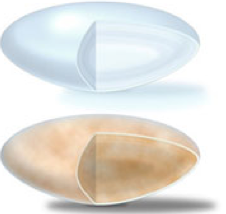
|
|
A cataract may not need to be removed right away if your lifestyle isn't significantly affected. In some cases, simply changing your eyeglass prescription may help to improve your vision. Contrary to popular belief, a cataract does not have to be "ripe" to be removed. However, once you are diagnosed with a cataract, your ophthalmologist needs to monitor your vision regularly for any changes.
CATARACT SURGERY FOR CLEARER VISION
When a cataract causes bothersome vision problems that interfere with your daily activities, your ophthalmologist may recommend surgery to remove the cataract. With cataract surgery, your eye's cloudy natural lens is removed and replaced with a clear artificial lens implant (called an intraocular lens or IOL).
You and your ophthalmologist can discuss the cataract surgery procedure, preparation for and recovery after surgery, benefits and possible complications of cataract surgery, cataract surgery costs and other important information. Together, you can decide if cataract surgery is appropriate for you.
CATARACT SYMPTOMS
Most age-related cataracts develop gradually. As a result, you may not notice signs or changes in your vision right away when cataracts first develop.
Gradually, as cataracts progress, you may have symptoms such as:
The only way to know for certain if you have cataracts is to have a dilated eye exam (where your pupil is widened with eye drops). Your ophthalmologist can detect early signs of cataract development by looking at your eye's lens.
Get a baseline exam at age 40 when early signs of disease and changes in vision may start to occur. Your ophthalmologist (Eye M.D.) will let you know how often you should return for follow-up exams. At any point, if you have symptoms or risks for eye disease, see your Eye M.D. Because your risk for cataracts and other eye diseases increases as you get older, starting at age 65 you should see your Eye M.D. every year. A complete eye examination will rule out any other condition that may be causing blurred vision or eye problems. Early detection and treatment of cataracts is critical to preserving sight.
Who Is at Risk for Cataracts?
Cataracts develop as part of the aging process, so everyone is at risk eventually. By age 75, about 70 percent of people will have cataracts. With age, our eye's lens slowly becomes less flexible, less transparent and thicker. Then areas of the lens become cloudy as protein in the lens begins to clump together.
Cataract risk factors
These factors increase your risk of developing cataracts:
If you have any of these risk factors for cataract, you should schedule an appointment with your ophthalmologist (Eye M.D.).
CATARACT CAUSES
The lens is made mostly of water and protein. As we age, the lens continues to grow layers on its surface and hardens. Protein in the lens may clump together and become cloudy in some areas, preventing light from passing clearly through the eye. This cloudiness of the lens is what we call a cataract.
If the clouding is mild or only involves a small part of the lens, your vision may be only slightly affected. If there is more clouding and it affects the entire lens, your vision will become severely limited and cataract surgery becomes necessary.
Less common types of cataracts, not related to normal aging, include the following.
This type of cataract can occur in infants or children. They may be hereditary or they can be associated with some birth defects. Some occur without any obvious cause.
These cataracts are caused by other eye diseases or previous eye surgery. Chronic disease can make you more likely to develop cataracts; for example, diabetes has been proven to increase risk for cataracts. Excessive use of steroid medications can spur development of this type of cataract as well.
These cataracts are related directly to an eye injury. Traumatic cataracts may appear immediately following injury, or they can develop several months or even years later.
CATARACT DIAGNOSIS
Slit-lamp exam
Your ophthalmologist will closely examine the eye’s cornea (see How the Eye Sees video above), iris, lens and the space between the iris and cornea. With this special microscope, the doctor is able to examine your eye in small, detailed sections, making it easier to spot abnormalities.
Retinal exam
When your eye is dilated, the pupils are wide open so the doctor can more clearly see the back of the eye. Using the slit lamp and/or an instrument called an ophthalmoscope, the doctor looks for signs of cataract. Your Eye M.D. will also look for signs of glaucoma and other potential problems with the retina and optic nerve.
Refraction and visual acuity test
This test assesses the sharpness and clarity of your vision. Each eye is tested individually for the ability to see letters of varying sizes.
Once I have a cataract diagnosis, what should I do?
CATARACT TREATMENT
If your vision is only slightly blurry, a change in your eyeglass prescription may be all you need for a while. However, after changing your eyeglass prescription, if you are still not able to see well enough to do the things you like or need to do, you should consider cataract surgery.
With cataract surgery, your eye's cloudy natural lens is removed and replaced with a clear artificial lens implant (called an intraocular lens, or IOL). Your ophthalmologist will discuss the cataract surgery procedure, preparation for and recovery after surgery, the benefits and possible complications of cataract surgery, cataract surgery costs and other important information.
Cataract surgery is often performed as an outpatient procedure and does not require an overnight hospital stay.
CATARACT SURGERY
With cataract surgery, your eye's cloudy natural lens is removed and replaced with a clear artificial lens implant (called an intraocular lens or IOL). Cataract surgery is often performed as an outpatient procedure and does not require an overnight hospital stay.
Pre-operative tests for cataract surgery
Before surgery, the length of your eye will be measured in what is called an A-scan, and the curve of your cornea will be measured in a technique called keratometry. These measurements help your Eye M.D. select the proper lens implant for your eye. You will also discuss the various lens options available to you.
If you have had previous LASIK or other laser vision correction, you can still have cataract surgery. In planning for cataract surgery, provide your Eye M.D. with the vision correction prescription you had before LASIK, if possible. This information will help your Eye M.D. calculate the correct IOL prescription for you. Previous refractive surgery can make determination of the correct IOL more difficult and your vision prescription prior to refractive surgery can help the surgeon calculate the correct IOL power.
Medications and cataract surgery
If you are having cataract surgery, be sure to tell your ophthalmologist about all medications and nutritional supplements you are taking. If you currently use or have ever used alpha-blocker drugs for prostate problems, such as Flomax®, Hytrin®, Cadura® or Uroxatral® , tell your Eye M.D. These medications may prevent your pupil from dilating properly during surgery, leading to possible complications. If your surgeon is aware that you have had these drugs, he or she can adjust their surgical technique to adapt as needed, allowing for a successful cataract removal procedure. You should also tell your Eye M.D. about any other sedative medications you are taking.
To reduce the risk of infection from surgery, your ophthalmologist may prescribe antibiotic eyedrops for you to use one or two days before surgery. 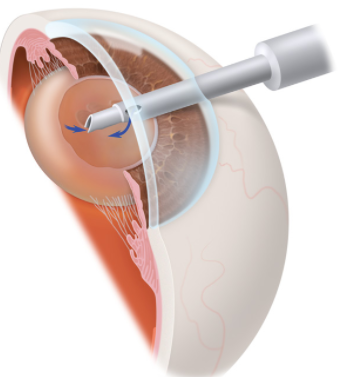
|
|
The cataract surgery procedure
The most common procedure used for removing cataracts is called phacoemulsification. A small incision is made in the side of the cornea (the front part of your eye), where your Eye M.D. inserts a tiny instrument that uses high-frequency ultrasound to break up the center of the cloudy lens and carefully suction it out.
After the cloudy lens has been removed, the surgeon will replace it with an intraocular lens (IOL) implant made of plastic, silicone or acrylic. This new, clear lens allows light to pass through and focus properly on the retina. The IOL becomes a permanent part of your eye. In most cases, the IOL is inserted behind the iris, the colored part of your eye, and is called a posterior chamber lens. Sometimes, the IOL must be placed in front of the iris. This is called an anterior chamber lens. When the IOL is in place, the surgeon closes the incision. Stitches may or may not be used. After the surgery, your Eye M.D. usually places a protective shield over your eye.
Cataract surgery recovery
You will spend a short period of time resting in the outpatient recovery area before you are ready to go home. You will need to have someone drive you home.
Following your surgery, it is very important to put in the eye drops exactly as prescribed by your ophthalmologist to promote healing. You will also need to take care to protect your eye by wearing the eye shield whenever you sleep, and by wearing special wraparound sunglasses in bright light. Be sure not to rub your eye.
During the first week of your recovery, you must avoid strenuous activity such as exercise or bending and heavy lifting (including anything over 25 pounds). You will also need to avoid getting any water, dirt or dust in your eye, which can lead to infection.
You may have some blurry vision a few days to weeks after surgery procedure. If you experience any pain or loss of vision, be sure to call your ophthalmologist.
Cataract surgery risks and complications
As with any surgical procedure, there are risks associated with cataract surgery. Risks and complications can include:
In some cases, the part of the lens covering that supports the IOL (called the capsule) can become cloudy several months or years after the first cataract was removed. This is called an "after cataract" or "secondary cataract." If this occurs and blurs your vision, your Eye M.D. will make an opening in the center of the cloudy capsule with a laser to allow light to pass through the lens properly again. This procedure, called a posterior capsulotomy, takes about five minutes in the doctor's office and requires no recovery period.
Most people who wear bifocals or reading glasses for near vision may still need to wear glasses after cataract surgery for reading, and, in some cases, even for distance. If you choose to have a multifocal or accommodative IOL, your dependence on glasses may be minimized or, in some cases, eliminated completely.
IOL IMPLANTS
Other important cataract lens replacement considerations